I am 25 years old, married for 5 years, unfortunately, God did not send us children. My husband and I were examined for a long time, everyone was looking for the cause of infertility. The doctors came to the conclusion that my husband and I were incompatible. Those. I can only get pregnant from him through artificial insemination. (What is meant by the word “incompatible”? When male reproductive cells enter a woman, they simply die there, not reaching their destination. And this only applies to my husband, since I can get pregnant from someone else. I have developed antibodies. And in order to avoid the environment in which sperm die, artificial insemination is needed.)
Unfortunately, today this is a very expensive procedure. I would like to ask whether it is possible to treat such a case with medication, how often do such cases occur, and whether in the future, if I do undergo artificial insemination, I will be able to conceive and give birth to a second or third child without the help of artificial insemination?
I would like to add that now there are a lot of married couples who do not have children and, perhaps, do not even suspect that they have the same problem as we do...
Vladislav

Unfortunately, infertility among married couples today is actually quite common.
This is not only a tragedy and a cause of disharmony in many families, but also a rather complex medical and social problem. A marriage is considered infertile if there is no pregnancy for 1 year among spouses of reproductive age who have regular sex life without the use of any contraception. Of course, such a formula is not a sentence or a diagnosis, but it is a good enough reason for a couple to think about it and begin to act.
 There are several types of female infertility. Until recently, the immunological infertility discussed in the letter was a mystery to doctors. For some time it was even classified as infertility of unknown origin, i.e. unknown origin. However, today all over the world and in our country they are quite successfully used latest methods immunological control and reproductive technologies, which not only make it possible to examine the family in detail, but also give spouses the joy of motherhood and fatherhood.
There are several types of female infertility. Until recently, the immunological infertility discussed in the letter was a mystery to doctors. For some time it was even classified as infertility of unknown origin, i.e. unknown origin. However, today all over the world and in our country they are quite successfully used latest methods immunological control and reproductive technologies, which not only make it possible to examine the family in detail, but also give spouses the joy of motherhood and fatherhood.
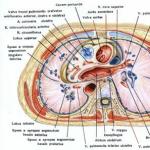
Biological or immunological incompatibility of spouses can lead to infertility in an absolutely healthy couple. Biological incompatibility tests are carried out 2 days before the upcoming ovulation and no later than 6 hours after sexual intercourse. A drop of mucus from the cervical canal is examined under a microscope to determine the number of active sperm in it. Normally, more sperm penetrate the mucus and remain motile. In case of immunological incompatibility or in case of violation of the properties of cervical mucus (after cervical surgery, hormonal disorders), spermatozoa are not detected in the preparation.
 The practice of drug treatment of immunological incompatibility of a couple exists: this is a course of treatment with antiallergic drugs (prescribed by a doctor on an individual basis) and the so-called condomotherapy - the recommended use of a pair of condoms for a period of at least three months. If, after such treatment, there are anti-sperm antibodies in the woman’s cervical mucus, the method of intrauterine insemination is prescribed, when sperm are injected directly into the uterine cavity. Thus, they will go through a “dangerous” stage of passage for them. In the event that the fertilizing ability of a man’s sperm is very poor or the incompatibility barrier cannot be overcome (when anti-sperm antibodies are present not only in the cervical mucus, but also in the woman’s blood, egg, follicular fluid), resort to artificial insemination with donor sperm. The principle of fertilization is similar. On a day of the cycle favorable for pregnancy, which is determined in advance according to ultrasound, RT, and the nature of the cervical mucus, processed sperm is injected into the woman’s uterus. Sometimes the attempt has to be repeated up to 2-3 times during the cycle. The effectiveness of intrauterine insemination is quite high.
The practice of drug treatment of immunological incompatibility of a couple exists: this is a course of treatment with antiallergic drugs (prescribed by a doctor on an individual basis) and the so-called condomotherapy - the recommended use of a pair of condoms for a period of at least three months. If, after such treatment, there are anti-sperm antibodies in the woman’s cervical mucus, the method of intrauterine insemination is prescribed, when sperm are injected directly into the uterine cavity. Thus, they will go through a “dangerous” stage of passage for them. In the event that the fertilizing ability of a man’s sperm is very poor or the incompatibility barrier cannot be overcome (when anti-sperm antibodies are present not only in the cervical mucus, but also in the woman’s blood, egg, follicular fluid), resort to artificial insemination with donor sperm. The principle of fertilization is similar. On a day of the cycle favorable for pregnancy, which is determined in advance according to ultrasound, RT, and the nature of the cervical mucus, processed sperm is injected into the woman’s uterus. Sometimes the attempt has to be repeated up to 2-3 times during the cycle. The effectiveness of intrauterine insemination is quite high.
 I would like to dispel the prejudice of readers regarding the unavailability of such treatment in Ukraine. Drug treatment of immunological infertility is carried out on the basis of regional reproductive health centers; the intrauterine insemination procedure is carried out in most regional specialized clinics. It should be noted that this procedure is simple - it does not require inpatient treatment on an outpatient basis, and it is relatively inexpensive. In addition, spouses who decide to resort to this method of treatment can count on some support from the state, because according to paragraphs. 5.3.6 clause 5.3 art. 5 of the Law, every taxpayer has the right to include in the tax credit of the reporting year the amount of expenses actually incurred for artificial insemination, regardless of whether he is married to the donor or not.
I would like to dispel the prejudice of readers regarding the unavailability of such treatment in Ukraine. Drug treatment of immunological infertility is carried out on the basis of regional reproductive health centers; the intrauterine insemination procedure is carried out in most regional specialized clinics. It should be noted that this procedure is simple - it does not require inpatient treatment on an outpatient basis, and it is relatively inexpensive. In addition, spouses who decide to resort to this method of treatment can count on some support from the state, because according to paragraphs. 5.3.6 clause 5.3 art. 5 of the Law, every taxpayer has the right to include in the tax credit of the reporting year the amount of expenses actually incurred for artificial insemination, regardless of whether he is married to the donor or not.
In a marriage, a child is not always born as quickly as the spouses would like. This is especially sad when both are young and completely healthy. Every third couple suffers from difficulties when trying to conceive. Such a problem must be dealt with, and for treatment it is necessary to establish its causes. Incompatibility of partners when conceiving a child is said to occur if, after twelve months of regular sexual activity, a woman does not become pregnant. The examination shows that the spouses do not have any pathologies. The lady does not take contraceptives, and the man does not use barrier contraception. Sometimes it happens that fertilization occurs, but after some time a miscarriage occurs.
Incompatibility of partners during conception: signs
The most obvious factor that catches your eye is the absence of children in a couple who have lived together for quite a long time and are absolutely healthy and prosperous.
A man and a woman are trying to conceive a child, but all their attempts end in failure. A year passes, and sometimes more, and the couple still has no offspring.
The main signs that indicate the presence of incompatibility between partners should be structured.
These include the following:
- xspouses regularly engage in sexual contact;
- both are completely healthy;
- they have been together for over a year;
- a woman cannot conceive, despite all attempts;
- no additional reasons interfere with the fertilization process;
- soon after conception, the fairer sex begins to menstruate;
- it happens to her;
- the woman is diagnosed, etc.
Causes of incompatibility during conception
The main factor leading to the inability to get pregnant against the background of general health is the influence various types functioning of the spouses' body. In a third of cases, difficulties lie in wait for the woman, in a third for the man, and in the remaining third for both partners. A small percentage of the probability is due to influence external environment.
Very often, the reason for the impossibility of fertilization is the couple’s too much desire, leading to nervous strain and physical exhaustion.
Most often, the main impetus for difficulties with conceiving and bearing a child are various pathological reactions of a woman’s lymphocytic system.
These include:
- immunological processes;
- Rhesus conflict;
- genetic reasons;
- mismatch between the microflora of the spouses.
Immunological infertility
One of the main reasons for this problem is immunological incompatibility. It lies in the fact that the fairer sex has an increased titer of antisperm antibodies that destroy sperm. Under such conditions, pregnancy becomes impossible.
Why this reaction develops, medicine is not always able to say with certainty. For some women this happens with every partner, for others - only with a certain one. It is not uncommon for a representative of the fairer sex to give birth to a completely healthy baby in her new marriage after living in marriage for many years and despairing of having a child.
Lack of love in a couple or a woman’s strong nervous tension also contributes to a negative response from her lymphocyte system.
Severe hormonal imbalances can sometimes lead to the development of such a pathology.
In cases where, even despite such a reaction of the female body, conception still occurs, it ends in miscarriage already in the first trimester. This immune reaction continues to affect the embryo.
In addition, the fairer sex has severe toxicosis, which directly indicates unfavorable processes in her metabolism.
Such factors put enormous pressure on the embryo, which cannot withstand such conditions. A miscarriage occurs.
In general, the mechanism of this process is identical to that which occurs during the development of allergies.
Therefore, before planning a pregnancy, it is necessary to take a test for the presence of antisperm antibodies in a woman.
It is also worth undergoing an examination of the ejaculate in order to make sure that its cells are completely viable.
Rhesus conflict
Most often, a woman and a man have a positive Rh factor. If the husband has a negative indicator, nothing terrible happens either. The problem occurs in fifteen percent of the fairer sex who have it.
A conflict arises when a woman has a negative indicator and a man has a positive indicator.
The blood protein becomes a kind of antigen, to which a woman begins to produce antibodies during pregnancy.
The process is as follows. The developing fetus develops a circulatory system. If unborn child inherited the father's indicator, then Rh conflict develops. It is closely related to the mother's immune system. The red blood cells of the embryo, captured by it, begin to be intensively destroyed. As a result, hemolysis develops.
Most often, spontaneous abortion occurs. The first pregnancy, as a rule, turns out to be normal; difficulties begin when you want to have a second child.
Therefore, women with a negative Rh factor are not recommended to have an abortion, since a new pregnancy will be fraught with enormous difficulties and great challenges.
Even if it persists and labor occurs, a dead or soon-to-be-dead baby is often born.
Therefore, a woman should be under close medical supervision, and shortly before the expected contractions she is given anti-Rhesus immunoglobulin, which helps reduce the allergic reaction. Such measures make it possible to reduce the activity of the immune system during childbirth.
Nowadays, such a situation is difficult, but completely solvable. Therefore, before planning a pregnancy, it is necessary to donate blood to identify the group and Rh factor. If incompatibility is diagnosed, the woman is constantly injected with a special immunoglobulin that suppresses the activity of lymphocytes. Sometimes a complete blood transfusion is recommended.
Genetic incompatibility
Typically, the embryo has a chromosome set inherited from each spouse. The difference is based on the presence of a specific antigen, Human Leucocyte Antigens (HLA), which translates as human leukocyte antigen. This is a special protein that attaches to the cell membrane. The more actively it is produced, the higher the likelihood of incompatibility between men and women.
When pregnancy occurs, the immune system of the fairer sex recognizes such a protein as foreign and begins to fight it. Most often, such a discrepancy leads to miscarriage. In cases where this does not happen, a baby may be born with severe developmental abnormalities.
Usually, gynecologists advise, when planning a conception, to immediately get tested for this indicator. It is detected in the blood. Most often, its presence is associated with the presence of autoimmune diseases or when the partners are related.
Microflora incompatibility
Each spouse's body has its own biocenosis, represented by a collection of microorganisms. They are classified as normal, opportunistic and pathogenic microflora.
However, those bacteria that do not cause any harm to their owner can trigger a powerful rejection mechanism in another person.
Therefore, partners need to pay attention to their feelings after sexual intercourse. If a woman experiences severe discomfort in the vagina or uncharacteristic discharge, this may be a sign of discrepancy in microflora indicators.
Sexually transmitted diseases are often the main cause of such problems.
This type of incompatibility is diagnosed very rarely and is usually detected no more than in two percent of cases.
The mechanism of its development is the same. A woman’s immune system reacts to the system of microorganisms in her partner’s genital area as a hostile environment. Therefore, spermatozoa, once in a woman’s vagina, are very quickly destroyed.
If you are planning a pregnancy, you should donate genital secretions for women and urethral secretions for men.
It is sown on a nutrient medium, and then the cells of the grown colony are examined under a microscope. A microbiological study is also carried out and the fact of incompatibility of the spouses is established.
What to do?
In order to avoid difficulties during conception, it is necessary to fully examine the body of a man and a woman for various factors. Since in all cases the cause of a negative scenario is the reaction of the immune system, we use special means to suppress it.
You should be especially careful if:
- one of the spouses suffers from unfavorable heredity;
- the father or mother of the unborn baby has already crossed the thirty-five year mark;
- the woman has already had miscarriages;
- partners are related;
- there is an unfavorable environmental situation in the area of residence;
- a couple who has been living together for a long time experiences persistent infertility;
- the family already had children with developmental anomalies;
- relatives of one of the spouses were diagnosed with autoimmune diseases, etc.
In some cases, partners are recommended to undergo IVF or ICSI. If people were late and the fact of discrepancy was discovered too late, it is sometimes recommended to terminate the pregnancy in order to avoid the birth of a child with severe malformations.
If measures are not taken, the immune system of the fairer sex will react to the husband’s body or to the developing fetus as an antigen with corresponding consequences.
Couple compatibility test for conceiving a child

There is a special study that allows you to evaluate the compatibility of partners.
To conduct a postcoital test, a woman gives a smear of mucus taken from the surface of the cervix. It will be studied for the degree of viscosity, level of crystallization and acidity of the medium. Upon contact with the spouse's ejaculate, it will be determined what reactions occur during their interaction.
The main requirements for the test are:
- Absence of intimate contact for at least three days;
- careful hygiene before engaging in sexual contact;
- absence of external influences on the internal genital organs after the end of intimate intercourse;
- it should not be accompanied by influence external factors or pharmaceuticals;
- before a sexual encounter, you should not use substances used for hygiene;
- after its completion, the woman should not get up for thirty minutes;
- It is advisable to see a doctor after seven to nine hours.
For additional research, both spouses need to donate blood and other biomaterial. He will undergo numerous immunological tests. If incompatibility is found for any factor, the doctor will prescribe appropriate treatment.
Due to the fact that this problem in couples is not so rare, medicine has developed special methods its corrections allowing them to have children.
Therefore, completely healthy partners who do not have offspring should not despair. It is necessary to contact specialists in time to conduct a comprehensive diagnosis and search for various ways to get out of this situation.
Nowadays, the incompatibility of partners when conceiving a child does not at all mean that they are sentenced to childlessness. There are numerous methods available to help people experience the joy of parenthood.
Usually, disappointing conclusions follow only in cases where they have put off visiting a doctor for too long and both are already well over forty years old.
Sometimes a completely healthy married couple cannot conceive a child for a very long time. Perhaps the culprit for this situation is the genetic incompatibility of husband and wife. In this case, the antigens of the future parents are very similar to each other. Oddly enough, such similarity from a genetic point of view is a negative factor.
This deviation in the interaction of antibodies does not allow carrying a child to term even in the case of successful fertilization: the pregnancy is terminated at the very early stages.
However, modern medicine has found ways to solve this problem. Therefore, when planning to conceive, it is imperative to consult an experienced geneticist. The doctor will prescribe genetic tests and, if necessary, appropriate treatment. After it, most spouses successfully become parents.
What is genetic incompatibility of spouses, what danger does it pose during conception? In order to answer this question, you need to know some structural features of human cells. Each of them has a special antigen on its surface - a protein called HLA. This abbreviation stands for human leukocyte antigen.
When pathogenic bacteria, viruses or even cancer cells enter the human body, the proteins immediately send a signal to the immune system. The immune response manifests itself in the immediate attack of “enemy” microorganisms with antibodies, the purpose of which is to eliminate harmful bacteria.
When conception occurs, the female body reacts to the fetus as a hostile element, because it also contains the genes of the father. However, simultaneously with this process, the body of the expectant mother triggers the production of antigens, which serve reliable protection placenta and embryo from the “army” of maternal immunity.
This protection scheme only applies in case of genetic compatibility, that is, if the genes of the parents have different structures.
If the husband’s leukocyte antigen is the same or very similar to his wife’s cells, then the female body does not produce protective bodies. Moreover, the presence of an embryo is perceived by him as his own “low-quality” cell, so the “army of defenders” does everything possible to get rid of the foreign object. This is the essence of genetic incompatibility.
 Pregnancies that occur due to genetic incompatibility very rarely end successfully. Most often it does not last more than 4 days. That is, a woman may not even suspect that conception has occurred, and takes the bleeding that occurs during a miscarriage as the beginning of the next menstrual cycle.
Pregnancies that occur due to genetic incompatibility very rarely end successfully. Most often it does not last more than 4 days. That is, a woman may not even suspect that conception has occurred, and takes the bleeding that occurs during a miscarriage as the beginning of the next menstrual cycle.
The genetic compatibility of spouses is fixed if the parents' chromosomes differ from each other. The more differences, the higher the chances of successfully conceiving and bearing a child. And, conversely, the more similar the chromosomes are, the more serious the issue of genetic incompatibility will be.
Is incompatibility curable?
There are very few cases where a complete gene match was diagnosed. And doctors have already learned to regulate the interaction of partially similar genes.
 A timely genetic study when planning a pregnancy will allow you to identify disorders and begin to correct them. In this case, therapy is carried out before conception, during it and during the first months of pregnancy.
A timely genetic study when planning a pregnancy will allow you to identify disorders and begin to correct them. In this case, therapy is carried out before conception, during it and during the first months of pregnancy.
After genetic compatibility tests have been taken, the doctor will analyze the results and prescribe the right type therapy. It will allow you not only to get pregnant quickly, but also to carry your baby to term without complications until birth.
The nature of the treatment will depend on how similar the genes are in the future parents. Sometimes it is prescribed to both spouses, and in some cases it is enough for only the expectant mother to undergo it. Medications administered intravenously to a woman help the immune system recognize foreign chromosomes and not kill them.
IVF or ICSI procedures may be offered as alternative treatments. However, you need to understand that each organism is individual, so you need to solve the problem in this way after consulting a geneticist.
Tests and genetic consultation
A consultation with a geneticist when planning a pregnancy necessarily includes an interpretation of the results of genetic tests. After all, only they can confirm or refute the diagnosis.
When planning a pregnancy, genetic tests are carried out about two weeks. For the study, you will need venous blood from two spouses.
Leukocytes are isolated from the blood using special reagents, because they contain the largest number of antigens. In this case, geneticists use the polymerase chain reaction method, which allows one to accurately determine the HLA phenotype.
Once the DNA analysis of each spouse is completed, they are compared. The presence of already two matches can become a factor that provokes permanent terminations of pregnancy or the inability to conceive.
Only a specialist in the field of genetics can decipher the results of such analyzes and draw conclusions about the presence of genetic incompatibility.
In medicine, there are cases where couples with genetic incompatibility successfully gave birth to healthy children without drug treatment. That is, if a woman managed to get pregnant and carry the baby for at least the first trimester, most likely she will give birth to him safely.
However, with such a diagnosis, it is better not to take risks, because very similar genes can cause various pathologies in the development of the fetus and lead to the birth of a sick child. Therefore, a full-type genetic blood test performed while planning a pregnancy can protect you from possible unpleasant surprises.
Treatment methods
Doctors learned how to safely maintain a pregnancy in such an unusual situation more than 30 years ago.
Several methods were used for this.
For example, a small piece of skin tissue was excised from a man and “implanted” into the body of his pregnant wife. The woman’s immune system continued to attack foreign cells. Only in this case, the role of the “stranger” was not the developing fetus, but the skin of the spouse. Also, to maintain pregnancy, the woman’s blood was “cleansed” of antibodies or the immunity of the expectant mother was reduced.
Modern medicine has in its arsenal safer and effective ways solving the problem of genetic incompatibility. One of the most popular methods is immunocytotherapy.
Immunocytotherapy for genetic incompatibility
The immunocytotherapy technique was developed and put into practice by Russian doctors. For many years now, with its help, many married couples have realized themselves as parents. The undoubted advantage of the technique is its effectiveness and the absence of complications after implementation. Moreover, it does not cause pain.
How does the procedure work?
 To carry out the procedure, you will need the spouse’s venous blood, from which leukocytes are separated. The resulting material is injected subcutaneously into the expectant mother.
To carry out the procedure, you will need the spouse’s venous blood, from which leukocytes are separated. The resulting material is injected subcutaneously into the expectant mother.
Red blood cells, which are removed from the husband’s blood, are responsible for determining the blood group and its Rh factor. The remaining leukocytes do not carry such an information load; they are neutral. Therefore, these indicators are not important for the procedure.
After the injection, a woman may feel slight redness and itching at the injection site. After a few days, the symptoms will disappear on their own.
As soon as the spouse’s lymphocytes penetrate the blood of the expectant mother, her immunity begins to intensively supply antibodies. They will become reliable protectors of the fetus and placenta from death in the future.
Stages of immunocytotherapy
Immunocytotherapy is carried out in several stages, each of which is necessary for an effective result.
First, the introduction of leukocytes is carried out according to the doctor’s recommendation;
The second injection is carried out 7 days after the first. Immediately after the procedure, the spouses need to begin conceiving;
The third stage of introducing the solution is carried out only when conception has occurred;
The last two injections will be prescribed individually by the gynecologist during the first trimester of pregnancy.
Contraindications
The immunocytotherapy procedure is safe and suitable for almost everyone.
The exception is couples who have suffered infectious diseases. For example, a spouse with a history of hepatitis will not allow this procedure to be performed. But even in this case, do not despair. An experienced doctor will not only tell you about possible contraindications to immunocytotherapy, but will also offer others, no less effective methods elimination of genetic incompatibility.
We can safely say that genetic incompatibility is not a death sentence. With the help of modern medicine methods and timely examination by an experienced geneticist, you can successfully become happy parents.
It happens: people have been married for more than one year, but there are no children. Both are healthy, sex is in perfect order, but pregnancy does not occur or the woman has miscarriages every now and then. And the problem lies in the incompatibility of the spouses, which prevents conception; This concept has many faces and does not interfere with understanding the details and assessing the chances of correcting the situation.
What is called incompatibility, what are its signs
Doctors explain the inability of a man and a woman to conceive a child with healthy reproductive organs and regular sex life without contraceptives due to the incompatibility of partners. This situation occurs often and sometimes breaks families.
According to statistics, up to 30 percent of cases of infertility are explained by disorders of the reproductive function of women, the same percentage is associated with male “failure”; The reasons for every tenth infertility remain a mystery to doctors. Incompatibility of partners accounts for 20–25 percent of cases.
Infertility or miscarriage, which may be caused by incompatibility, is diagnosed when:
- a couple is trying to conceive a child, but the woman has not become pregnant for more than a year; in this case, the spouses are healthy or have diseases that do not affect conception;
- the woman had several miscarriages in the early stages - however, in the first weeks of pregnancy it is difficult to determine, since the embryo is too small for its rejection to be noticed; a woman mistakes a miscarriage for normal menstruation;
- Several times doctors diagnosed a frozen pregnancy - when the fetus died in the womb.
 Thoughts about possible infertility come to mind when, after a year of married life, you are still unable to conceive a child.
Thoughts about possible infertility come to mind when, after a year of married life, you are still unable to conceive a child. In some cases, it even comes to childbirth, but the baby is born with severe genetic abnormalities (Down syndrome, Edwards syndrome and others).
Types of incompatibility
The basis of each type of incompatibility is the pathological reaction of the female body to changes associated with conception and gestation.
The following are to blame for failures when trying to conceive a baby:
- Rhesus conflict;
- immunological factors;
- contradictory microflora of spouses;
- genetic inconsistencies.
Rh factor conflict
The blood protein that attaches to the surface of red blood cells - erythrocytes - is called the Rh factor. However, not every organism has such an element. There is protein - it means Rh positive; no protein - Rh factor negative.
A Rh conflict after conception can only arise if the expectant mother has Rh negative blood, and the future dad has Rh positive blood. But this is not a verdict either, because:
- in half of the cases the baby will inherit a negative Rh factor from the mother - which means there will be no conflict;
- even when the child has paternal Rh-positive blood, conflict rarely occurs during the first pregnancy (if the woman has not had an abortion before, she has not had miscarriages).
The mechanism is this: the baby’s positive blood is unfamiliar to the mother’s body, which mistakes the Rh factor for an “aggressor” and begins to produce antibodies for its own protection. However, during the first pregnancy, the immune system does not have time to produce antibodies, because during a normally ongoing pregnancy negative blood the fetus does not enter the mother's body. Only during childbirth does the blood of mother and child mix.
So during the second pregnancy, maternal antibodies are at the ready and, if the embryo again has Rh-positive blood, they attack the “enemy”. Antibodies destroy the baby’s red blood cells, which is why he often dies.  In case of Rhesus conflict, under the influence of maternal antibodies, red blood cells - erythrocytes - are destroyed in the fetus
In case of Rhesus conflict, under the influence of maternal antibodies, red blood cells - erythrocytes - are destroyed in the fetus
When a woman has positive Rh and the child has negative Rh (inherited from the father), “blood enmity” is excluded; The Rh factor protein is familiar to the mother's body, and the fact that it is absent in the blood of the fetus is tolerated by the immune system calmly.
Some Rh-negative mothers with Rh-conflict in the body manage to carry the child to birth - under the close supervision of doctors. But it is possible that the baby will die during childbirth or suffer complications in the form of anemia, jaundice, and edema. To reduce the threat of irreversible consequences, the expectant mother:
- starting from the 28th week, anti-Rhesus immunoglobulin is administered;
- do a blood transfusion.
To prevent the Rh conflict from canceling out the parents’ plans for the birth of a second child, after the birth of the first child, the mother is given an injection of immunoglobulin (within three days); This is a deception drug that imitates the fight against “aggressors” by calming the immune system. If she is pregnant again, she will no longer be “excited”, recognizing the Rh factor.
Immunological (biological) incompatibility
By the way, Rh conflict is one of the types of such incompatibility. Let's consider another one.
It happens that the female body mistakes sperm for foreign objects; as a result, the production of antibodies is enhanced, which destroy male germ cells before fertilization. Moreover, for some women this happens with every partner, while for others - only with a specific one. Medicine finds it difficult to explain why.
Sperm also sometimes contains antibodies that kill germ cells - this is a kind of allergic reaction of the male body to its own seminal fluid. Even if some of the sperm survive and reach the egg, there is a high probability that the pregnancy will be terminated.
Factors provoking immunological infertility:
- weak immunity in partners or one of them; caused by advanced infections, bad habits, and, in women, by repeated abortions;
- many casual relationships in the past with one or both partners;
- long-term use of condoms in intimate life - they spoil the seminal fluid;
- the nervous tension that a woman feels leads to increased activity lymphocytes - immune cells;
- hormonal imbalance in the female body.
When, despite obstacles, conception still occurs, the aggressive immune system does not calm down until it destroys the embryo. The severe toxicosis that accompanies the body’s negative reaction also contributes to this outcome.  One of the consequences of the immune conflict in the female body after conception is severe toxicosis, in which the tissues of the embryo are poisoned
One of the consequences of the immune conflict in the female body after conception is severe toxicosis, in which the tissues of the embryo are poisoned
An experienced doctor will help eliminate immunological problems with conception (although treatment is not effective in every case). Prescribed:
- immunostimulants - drugs to increase the body's protective properties; The doctor will tell you which ones to use, but as soon as the woman finds out that she is pregnant, she must stop taking the medications, otherwise the strengthened immune system will “revolt” against the embryo;
- antihistamines - to combat allergies;
- corticosteroids (one week before ovulation); Adrenal hormones increase the body's resistance to infections and inflammation.
Until the expected conception, spouses need to use condoms.
If therapy does not help, doctors advise resorting to IVF or intrauterine insemination - the introduction of the husband's seminal fluid into the uterus.
Microflora incompatibility
The microflora of each person is individual; Both beneficial and opportunistic bacteria live in the reproductive organs, but the microbes normally do not harm the host organism. But the microflora of the female genital tract sometimes tries to reject foreign objects (spermatozoa). By the way, the cause of such incompatibility may be a sexually transmitted infection in one of the spouses.  The microflora of a woman’s genital organs sometimes reacts with hostility to the invasion of male reproductive cells and kills them; conception becomes impossible
The microflora of a woman’s genital organs sometimes reacts with hostility to the invasion of male reproductive cells and kills them; conception becomes impossible
Symptoms of microflora mismatch in a woman after sexual intercourse:
- discomfort in the vagina;
- unusual vaginal discharge.
Candidiasis and genitourinary inflammation often appear. After diagnosis, the doctor selects antibiotics for each partner; As a rule, therapy gives results.
This type of infertility is rare - only two percent of couples trying in vain to conceive a child.
Genetic incompatibility
This is what they call a conflict at the chromosome level; caused by the similarity of leukocyte antigens (HLA) - proteins that are attached to cell membranes.
When the spouses have different antigens, the maternal body acts in two ways during embryo implantation: it produces antibodies against the paternal antigens present in the embryo, but at the same time supplies the baby with antigens that protect it from antibody attack.
When the male leukocyte antigen is similar to that of the partner, the situation changes. A woman’s body perceives the embryo as its own “damaged” cell, something like a malignant formation that needs to be destroyed. The unequal struggle quickly ends with the death of the embryo: miscarriage, frozen pregnancy. As a rule, everything happens within four days after conception.
If the embryo still survives, the risk of having a baby with severe chromosomal abnormalities is high.
Complete genetic incompatibility is extremely rare - mainly when spouses are close relatives and have identical sets of chromosomes. Here medicine is still powerless. In case of partial incompatibility, spouses are advised to:
- immunocytotherapy before conception - the introduction of the husband's lymphocytes into the woman's blood; the antibodies produced in response to this will protect the embryo in the future;
- medications that, when administered into a vein, help women’s immunity to respond correctly to a similar antigen;
- conception using IVF.
Tests for suspected incompatibility
To identify this type of infertility, the couple needs to undergo an examination; In each situation, certain tests are taken, which are usually prescribed by a fertility specialist. In addition, a woman visits a gynecologist, and a man visits a urologist.  In order for the family to finally have offspring, the infertile couple will have to go to the doctors and have a lot of medical procedures, but the efforts are usually rewarded
In order for the family to finally have offspring, the infertile couple will have to go to the doctors and have a lot of medical procedures, but the efforts are usually rewarded
If doctors suspect that the conflict is immunological, patients are recommended a so-called post-coital test: in the laboratory they study biomaterial in the form of mucus taken from the cervix after sexual intercourse. Normally, the number of dead and surviving sperm should be equal; if there are more dead, there is an immune contradiction.  The ratio of live and dead sperm in the cervix during a post-coital test will show whether there is immunological incompatibility between partners
The ratio of live and dead sperm in the cervix during a post-coital test will show whether there is immunological incompatibility between partners
Conditions for the analysis:
- three days before control intercourse, avoid sexual intercourse;
- 9–12 hours before submitting the biomaterial for examination, sexual intercourse takes place (and no stimulants like Viagra, otherwise the test result will be distorted);
- before the “procedure” a woman should not wash herself or douche;
- To ensure that enough seminal fluid is retained in the cervix, after contact it is better for the woman to remain in a horizontal position for about half an hour.
This test is not easy to pass. A good friend of mine, who passionately wanted a child from her new husband, could not get pregnant (it was approaching forty). Among other tests, she was prescribed a postcoital test. “You try to do it according to instructions,” a friend complained to me, “we do it this way and that - nothing works out. As a result, we can no longer look at each other.” What do you think - the laboriously obtained and finally submitted sample was rejected in the laboratory; There was no longer enough strength for new “torment,” so they had sex solely out of inspiration, without preparation or precautions, and the woman decided to give birth with the help of IVF. Several rejections, one ectopic - and finally it happened; Now my friend is a happy mother of her second daughter and for the rest of her life she will remember how difficult it was for her.
To confirm the Rh conflict, both spouses donate blood to determine the group and Rh factor (if they have not already done so). The doctor writes a referral; blood is donated from the ulnar vein on an empty stomach.  Such a blood characteristic as the Rh factor does not change throughout life, so it is enough to determine it once
Such a blood characteristic as the Rh factor does not change throughout life, so it is enough to determine it once
The immunological incompatibility of spouses is manifested in the formation of antisperm bodies, which can completely immobilize sperm and cause them to stick together. Also, the cause of infertility can be a woman’s allergy to sperm.
Recently, infertility has become very common among married couples. The reasons can be quite different and many of them can be successfully treated. And only in 10 percent of all cases of infertile marriages are both spouses considered completely healthy, without any diseases that could prevent them from having offspring. Moreover, both spouses can have their own children, but from other partners. In such cases, immunological incompatibility of partners is most often diagnosed.
This incompatibility manifests itself in the formation of antisperm bodies, and they can form in both men and women. As for men, autoantibodies to sperm are formed in the seminal plasma, resulting in their autoagglutination, that is, gluing. In women, antibodies are formed as a result of the penetration of surface and intracellular sperm antigens, sperm enzymes, as well as blood group antigen of the ABO, MNSS, Rh-Hr system, antigen of the HLA histocompatibility system, which are contained in sperm, into the secretion of the female reproductive system. Antibodies are synthesized in the mucous membrane of the cervical canal, in the endometrium and fallopian tubes. As a result of contact, they are able to completely immobilize sperm and cause them to stick together.
In addition, an autoimmune or allergic reaction to the antigens of the corresponding follicular fluid and the pellucida of the follicle may occur in a woman’s body. Investigating the cause of immunological infertility, we can say that the main reason for the childlessness of a particular couple is the woman’s allergy to sperm or other components of the partner’s sperm.
There are several ways to diagnose immunological incompatibility. If the couple has no other causes of infertility, then tests and special tests are used. The main method is to collect biological material from spouses and conduct tests to assess sperm activity in cervical mucus.
The following tests are popular in modern medicine:
- postcoital test “Shuvarsky-Guner”;
- Kurzrock-Miller test;
- Izojima test.
 These experiments are carried out during the period of ovulation; in addition, it is recommended to stop taking any drugs for a while. medicines so that the test results are reliable. As for training men, it is most often recommended to adhere to general rules used when taking a spermogram. You should not drink alcohol, take medications, or visit the sauna, as this can negatively affect the qualitative and quantitative characteristics of sperm.
These experiments are carried out during the period of ovulation; in addition, it is recommended to stop taking any drugs for a while. medicines so that the test results are reliable. As for training men, it is most often recommended to adhere to general rules used when taking a spermogram. You should not drink alcohol, take medications, or visit the sauna, as this can negatively affect the qualitative and quantitative characteristics of sperm.
Postcoital test
It is carried out in the middle of the menstrual cycle, during the period of expected ovulation. Required condition The post-coital test must include the presence of sexual intercourse, in which the man's sperm enters the vagina. After 2-3 hours, secretions from the cervical canal and posterior vaginal vault are collected, and then the behavior of sperm is examined. If sperm make oscillatory movements instead of forward ones, this indicates that there are anti-sperm antibodies in the cervical mucus. Next, a quantitative assessment of the sperm in the field of view is carried out under a microscope. If more than 10 motile sperm are detected, the test is considered positive; if less than 10, the test results are questionable and may be the reason for a repeat test. But if sperm are absent or motionless, or make pendulum-like movements, the test is considered negative.
Kurzrock-Miller test
This method also consists of examining the biomaterial of the spouses, but unlike the Shuvarsky-Guner test, the material is taken separately from each spouse.
This method also allows you to preliminarily determine the quality of the taken material. After all, the behavior of the sperm can be influenced by factors such as increased acidity or alkalinity of the environment, viscous or too thick mucus, dead epithelial cells create an obstacle to the movement of sperm, low sperm morphology and too viscous ejaculate mass. Before performing the Kurzrock-Miller test, it is very important to exclude extraneous factors, such as the presence of hidden inflammatory processes, in a couple, as this may affect the reliability of the result.
This type of test is carried out using the direct or cross method.
The direct method involves testing the interaction of a woman's cervical mucus and a man's sperm, which are combined in a test tube. And cross-testing involves the use of biomaterials from donors who have their own children.
The material is taken from the woman on the day when ovulation occurs. The slime is placed on glass and covered with another glass on top. The biomaterial of the partner and the donor is placed into the resulting gaps. Sperm interacts with mucus at a temperature of 37°C for six hours. Experts periodically monitor the process through a microscope. Qualitative characteristics The spouse's sperm are detected in the same way, using the cervical fluid of the spouse and a healthy female donor. To ensure the reliability of the result, the couple should stop having sex a few days before submitting the materials; it is also recommended to stop using medications that may affect the test results.
 The result is considered positive if the sperm do not die during the interaction of the biomaterial and remain mobile. A result in which natural conception is impossible due to low quality sperm or the peculiar properties of cervical mucus is considered negative. Depending on the behavior of the sperm, specialists can make recommendations for further treatment.
The result is considered positive if the sperm do not die during the interaction of the biomaterial and remain mobile. A result in which natural conception is impossible due to low quality sperm or the peculiar properties of cervical mucus is considered negative. Depending on the behavior of the sperm, specialists can make recommendations for further treatment.
This test is also carried out on the day of ovulation, but in addition to cervical mucus and ejaculate, the partners’ blood serum is also taken to determine serum spermommobilisins. Sperm-immune human serum is used as controls. Blood serum guinea pig serves as a source of compliment. In it, as well as in normal human serum, 90% of sperm are immobilized at a certain temperature. The test blood sera of the woman and her partner are also inactivated. The test gives correct results only if the spouse’s sperm meets the norm in terms of its characteristics.
When calculating the results, the number of moving spermatozoa after exposure to ejaculate plasma, test blood serum and endocervical mucus is taken into account. The sperm immobilization coefficient will be positive if it is more than two units.
Unfortunately, the immunological form of infertility has not been well studied today and is big problem for the whole world, since the reason for the appearance of antibodies that fight sperm has not yet been established. Treatment is not always successful and leads to conception and successful birth of a child.
In case of immunological infertility, the content of T-helpers increases and the level of T-suppressors decreases, which leads to an increase in the immunoregulatory index.
However, several methods have been developed to treat immunological infertility. One of them is the subcutaneous injection of the husband's lymphocytes under the skin of the wife, which triggers the normal immune mechanism and prepares him for pregnancy.
Treatment of immunological incompatibility
As already noted, treatment of immunological infertility is ineffective, but there are still several methods that in some cases help to cope with the problem.
First method – This is the conduct of condom therapy for six months or more in order to reduce sensitization in a woman’s body. The principle of therapy is based on stopping unprotected sexual intercourse.
Second method – this is the administration of varying doses of corticosteroids over several months or a week before ovulation .
TO third method include desensitization antihistamines, such as tavegil, zyrtec (cetirizine), loratadine.
Successful results can also be achieved with the use of immunostimulants or an intrauterine partner or donor.