The nature of epidemics usually takes on those diseases that are quickly and easily transmitted from person to person. Main distribution routes infectious diseases: - through food, water or household contacts (dysentery, typhoid fever, etc.); - airborne droplets (for example, influenza); - through blood-sucking insects(malaria, typhus); - contact route: through blood and other fluids (AIDS, rabies). There is also the concept of mental epidemics, that is, the widespread spread of certain mental illnesses. This usually happens on the basis of religious or revolutionary movements. The reasons for their occurrence are superstitions, suggestion or self-hypnosis, the desire to follow the leader or simply the majority. So a large number of people may experience hallucinations, visions, seizures, attacks of hysteria, outbursts of aggression, and suicidal tendencies. An example is the dance of St. Vitus, an epidemic of which appeared in end of the 14th century century. As for infectious natural diseases, their causes are varied and not fully understood by scientists. The occurrence of epidemics can be influenced by many factors, overlapping each other. So, there is a version that abnormal heat leads to activation of the influenza virus. Scientists have been thinking about the causes of epidemics for a long time. Even in ancient Egypt, the idea of natural disasters as a cause of natural diseases arose. Russian scientist A.L. Chizhevsky cosmological theory, according to which global processes occurring on Earth (wars, crises, epidemics) are subject to cycles of solar activity. Both socio-economic theories (David Ricardo) and ethical-cultural theories (Albert Schweitzer) were put forward. Epidemics in human history are mainly problems of cities, since in crowded conditions contact with the virus is more likely. If you add to this poverty and unsanitary conditions, you get ideal conditions for an epidemic to occur. An example of this is Europe in the 14th-17th centuries, when sewage spilled out of windows directly onto the street. The plague of 1665 killed a third of London's population. Scientists suggest that the disease originated in Central Asia, reaching Milan with ship rats. People blamed Jews, witches, or their own sins for their troubles, until the number of rats and the fleas that lived on them fell. Outbreaks of the plague receded - this happened at the end of the 17th century. Nowadays, when sanitary conditions have improved significantly, epidemics are not a thing of the past (influenza, AIDS), and scientists still have not come to a consensus on methods of combating them. Some people hope for advances in medicine, while others look for the roots of the disease in the spiritual crisis of humanity. New problems have also arisen, for example, in highly developed countries, cardiovascular diseases have become epidemic.
Epidemic is the rapid spread of an infectious disease among the population, significantly exceeding the normal incidence rate for a given area. Progresses over time and can become a source of emergency not only in a certain locality, but also on the territory of several countries.
Fighting epidemics as natural disasters has been and remains a difficult task. Despite all existing measures to prevent the spread of diseases, the number of victims of infection can amount to millions of people. An example is HIV infection, which has spread to all countries of the world. Each new outbreak may differ significantly from previous ones. The course of the epidemic is influenced by climate and weather conditions, geographical location region, as well as household and hygienic conditions residence of residents.
The science of epidemiology - what does it study?
Epidemiology is a science that studies and describes the patterns of occurrence and spread of diseases, as well as ways to combat them and preventive measures.
Epidemic process
An epidemic process is the continuous spread of an infectious disease that occurs when three conditions are met:
- presence of a source of infection;
- transmission mechanism;
- people susceptible to infection.
The absence of at least one of these conditions leads to a disruption of the chain of the epidemic process and stops the transmission of the disease.
At the same time, the occurrence of the epidemic and the nature of its course are also influenced by natural conditions(presence of natural foci of infection), social factors and the state of the health care system.
The beginning of an epidemic is impossible without a source of the disease, where the pathogen multiplies and accumulates. This source is an infected person or animal. Moreover, transmission of the disease is possible not only during an acute condition, but also during the period of recovery and carriage. Even when the main symptoms of the disease have subsided and health has improved significantly, microbes continue to be released from the body. Objects of the environment (for example, personal items - dishes, towels, etc.) can also serve as a source of disease, because the pathogen is present on them, albeit for a limited period of time.
Spread of the epidemic
The spread of epidemics occurs through certain mechanisms of pathogen transmission from the source of infection to a sensitive organism.
The release of microbes is short-lived and is accompanied by the release of one or another substance. For example, droplets of saliva when coughing or sneezing. Once in the environment, the pathogen is transported further with the help of air, water, food, household items, soil, and living carriers - insects and animals. After which it penetrates into a healthy but sensitive body.
Any infectious disease is characterized by its own transmission mechanism, which was formed as a result of evolution. Depending on the location and reproduction of the pathogen in the infected body, as well as transmission factors, four main mechanisms are distinguished:
- Aerosol;
- Fecal-oral;
- Transmissible;
- Contact.
With the aerosol transmission mechanism, epidemics spread through the air. The pathogen is released in external environment when talking, coughing or sneezing in the form of an aerosol and can easily move inside the room and even penetrate through corridors and ventilation ducts beyond its boundaries. In this way, the epidemic of influenza and childhood infections is supported: measles, chickenpox, whooping cough.
Severe epidemics of intestinal infections (for example, cholera) are caused by the fecal-oral mechanism of transmission of the pathogen. The feces of a sick person entering the water contaminate it, which contributes to the further spread of the disease.
The vector-borne mechanism of infection transmission (through insects) underlies the spread of epidemics of the disease that has become the most terrible in the history of mankind - the plague. Insects and animals also serve as vectors for many other infectious diseases found throughout the world. For example, epidemic typhus is transmitted to humans through lice bites, and malaria is transmitted to humans through mosquito bites.
The contact transmission mechanism contributes to the development of diseases of the skin and mucous membranes, including sexually transmitted diseases. This transmission mechanism should not be underestimated, because one of the most dangerous infections in modern society, HIV, is transmitted from person to person through sexual contact.
End of the epidemic
The natural end of an epidemic occurs when all susceptible people have been infected and recovered from the disease, acquiring immunity. For example, according to this scenario, a gradual decline in the incidence of influenza develops. People with weakened immune systems are most susceptible to this respiratory virus: children, pregnant women, the elderly, and those suffering from chronic diseases if they have not been vaccinated beforehand. After the “wave” of an infectious disease has swept through the most vulnerable groups of the population, the epidemic gradually subsides.
The epidemic can be put to an end using various control methods aimed at all parts of the epidemic process.

The set of various scientifically based methods of combating epidemics and prevention measures is called anti-epidemic measures. Thanks to them, it is possible to prevent the development of infectious diseases among the most vulnerable groups of the population, reduce the overall morbidity rate in the country, and even completely eliminate certain diseases.
Anti-epidemic measures affect one or more parts of the epidemic process:
- The source of the disease is restrictive measures;
- Transmission mechanism – disinfection;
- Body susceptibility – immunoprophylaxis.
Active measures aimed at combating an infectious disease lead to the end of the epidemic.
Restrictive measures
Epidemic control measures, aimed at limiting the source of the disease, are introduced when cases of highly contagious infectious diseases are identified among the population that are spreading within a specific area, for example, a city.
There are two options for restrictive measures:
- Quarantine;
- Observation.
The well-known word “quarantine” can often be heard in news releases, especially during periods of increasing flu incidence. It implies measures that prevent the spread of a dangerous infectious disease among the population, in other words, the development of an epidemic. Quarantine is essentially the isolation of sick people (the source of the disease).
Observation, on the contrary, involves isolating a group of healthy people who have been in contact with sick people or carriers of infection. This is necessary for medical observation, control and, if necessary, treatment in order to prevent the onset of an epidemic or its spread.
Disinfection
The spread of the epidemic is impossible if the mechanism of transmission of infection is broken. This is facilitated by compliance with general sanitary and hygienic rules, including personal hygiene rules, as well as disinfection. Of course, for every infectious disease, certain disinfectants are effective, which are selected depending on the properties of the pathogen and its resistance.
There are two types of disinfection:
- Routine disinfection is carried out at the patient’s place of residence if his treatment is carried out on an outpatient basis. It can be carried out, for example, by relatives, following the instructions of medical personnel;
- Final disinfection is carried out after hospitalization.
Immunoprophylaxis
To prevent infectious diseases and their active spread among the population, essentially epidemics, immunoprophylaxis (preventive vaccinations) is carried out.
Vaccination of residents in various countries is carried out in accordance with the national calendar of preventive vaccinations. IN Russian Federation it is approved by the Ministry of Health. It contains: a list of infectious diseases, timing of vaccination against them, as well as categories of people who should be vaccinated. The first part provides information about mandatory vaccinations, and the second - those performed only for epidemic indications.
The fight against epidemics begins with prevention - early immunization of the population.

Various evidence of horrific pandemics that caused the devastation of vast territories has survived to this day. Traces of some infectious diseases have been found in ancient burials. For example, signs of leprosy and tuberculosis have been found on Egyptian mummies. The symptoms of many now known diseases are described in the manuscripts of ancient civilizations.
The first epidemic, which is called the “Justinian Plague,” began during the reign of the Byzantine emperor Justinian I. It covered the entire known territory of the world at that time and lasted for two centuries (541-750), appearing in the form of individual outbreaks.
According to surviving chronicles, the source of the first epidemic arose in Egypt. Along trade routes, the infectious disease was brought to Constantinople, and then spread throughout the territory of Byzantium and spread to neighboring countries.
More than 100 million people worldwide became victims of the first epidemic.
Plague epidemics
Long before the advent of scientifically based measures to combat the spread of epidemics, people in medieval Europe began to detain people at border points for a period of 40 days to prevent the plague. Thus, “quarantine” arose, a term that Italian language literally means "forty days".
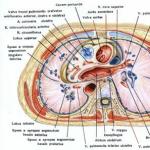
Plague is an acute infectious disease that belongs to the group of quarantine diseases. It is extremely difficult. Accompanied by fever, general intoxication of the body, damage to internal organs, primarily the lungs and lymph nodes.
In natural foci, the existence of infection is maintained by small rodents - marmots, gophers, rats and others. The disease is transmitted by fleas. The most common forms of plague are bubonic and pneumonic.
Plague is strongly associated with epidemic death dangerous disease. Indeed, the most famous plague epidemic, which claimed the lives of 60 million people, became one of the worst in human history and was called the “Black Death.” Presumably its appearance is a consequence of climate cooling, which attracted rats to human habitation. In 1320, the first cases of the disease were noted. First, the plague epidemic swept through China and India, and then spread to the Don and Volga rivers. From there the disease spread to the Caucasus and Crimea and was later transported to Europe.
The last plague epidemic recorded in the world was in 1910 in Manchuria. According to various estimates, its victims were from 60 to 100 thousand people. In Russia, emergency measures were taken to counter the epidemic, in particular, sanitary conditions were improved, deratization was carried out (extermination of rats) and a new hospital was equipped in Irkutsk. Properly carried out anti-epidemic measures made it possible to prevent the further spread of infection.
Risk of getting plague in the 21st century
Episodes of human plague infection are recorded almost every year. This is not surprising, because natural foci of this disease exist not only in Asian and African countries, but also in Russia, for example, on Lake Baikal.
However, the risk that a plague epidemic will occur these days is minimal, and there is no need to be afraid of it. Until the 1970s, the Soviet Union carried out massive measures to treat natural foci to reduce the number of rodents. Currently, constant monitoring is carried out by anti-plague brigades.

Smallpox, or smallpox, is a highly contagious viral infection. In the 16th century, Spanish conquistadors brought the disease to America. The Aztec Empire then occupied the Mexican Yucatan Peninsula and had a population of several million people. At the end of the epidemic, after an encounter with a previously unknown microbe, the number of residents was halved.
In Russia, smallpox was first recorded at the beginning of the 16th century. The infection was brought to Siberia. After the epidemic, the population decreased threefold. In Europe, even in the 18th century, half a million people died annually from a dangerous disease.
In the late 1970s, WHO named smallpox the first infection to be completely eradicated thanks to worldwide vaccination. Since then, not a single case of the disease has been recorded.
Cholera epidemics
Cholera is an intestinal infection that leads to a sudden loss of fluid - dehydration of the body. The spread of the disease occurs through contaminated water or food.
Ganges River in India - natural hearth cholera. The humid and warm climate, non-compliance with sanitary and hygienic standards, and a large number of inhabitants support its existence. The first cholera pandemic began in India. From 1817 to 1926 There have been six cholera pandemics. They covered countries Southeast Asia, Africa, Europe and America. In Russia, the cholera epidemic of 1830 became the first large-scale intestinal infection. The pathogen was brought into our country from Afghanistan, Iran and Turkey.
Despite the fact that there is currently etiotropic treatment for cholera (antibacterial drugs), the mortality rate is 5-10%, primarily due to dehydration.

Epidemic typhus is an infectious disease that is accompanied by damage to the central nervous system (central nervous system), the vascular bed, and the appearance of a specific rash.
The source of infection is an infected person who has the pathogen in his blood. The transmission mechanism is transmissible - through vectors - head and body lice. Insects acquire the infection by sucking blood and after 5 days are able to spread it further. The person begins to mechanically scratch the site of the bite, thereby rubbing lice excrement into the wound, which promotes infection.
Typhus is called a disease of wars and natural disasters. The fact is that the spread of the epidemic is facilitated by unsanitary conditions - the inability to comply with sanitary and hygienic rules.
In the period from 1805 to 1814. A typhus epidemic swept across Europe. The French army was in a difficult situation on its retreat from Russia. Soldiers were left in different cities (including Smolensk and Vilno), which led to the spread of an infectious disease.
The fight against typhus epidemics should begin with the destruction of lice, in other words, disinfestation. The spread of the disease is also stopped by introducing quarantine - isolating patients.

HIV infection is a sluggish, fatal disease caused by the human immunodeficiency virus. It affects the cellular part of the immune system - T-helper cells (CD4), resulting in the development of secondary immunodeficiency. The body becomes virtually defenseless against a wide variety of microbes. Infectious diseases arise, including those that are not typical for people with a normally functioning immune system.
HIV epidemic in the world
The HIV epidemic became known to the whole world in the late 1970s, when the disease spread across African countries. In Europe, it was possible to keep the situation under control until the end of the 1990s, when the total number of infected people almost tripled.
According to WHO, in 2015, 36.7 million HIV-infected patients were registered in the world. In total, more than 70 million people have been infected since the beginning of the epidemic.
According to statistics, the region with the highest mortality rate from HIV infection is Africa. The regions with the highest scores also include: Central Asia and Eastern Europe.
Treatment of HIV infection currently remains a challenge. There is still no medicine that can kill the virus in the human body. The mortality rate from AIDS, as the last stage of the disease, is 100%. The HIV epidemic has been sustained for many years precisely because of this fact.
According to the UNAIDS (Joint United Nations Program on HIV/AIDS) strategy, it is possible to stop the HIV epidemic by 2030. A big role is given to informing the population about preventive measures and treatment methods.

The first case of HIV infection in the Soviet Union was registered in 1986. In the early 1990s, the collapse of the country led to disruption of the epidemiological service and actually contributed to the development of the HIV epidemic in Russia.
According to the results of 2015 presented by UNAIDS, the HIV epidemic in Russia continues. The rate of increase in incidence in our country is ahead of most other countries in the world, including the African continent.
The most tense situation regarding the incidence of HIV/AIDS in Irkutsk region, where almost every second person out of a hundred has a diagnosis confirmed by special tests.
It is believed that the main reason for the deterioration of the situation in Russia is due to the lack of preventive measures, as well as the low provision of antiretroviral therapy to infected people. According to the Ministry of Health, only 37% of patients who are under constant supervision receive the necessary medications.
Another reason for the spread of the HIV epidemic in Russia is the increase in the number of injection drug users. After all, the use of intravenous drugs with unsterile syringes is the main route of transmission of infectious diseases.
The HIV epidemic in Russia can be stopped if the promotion of preventive measures is strengthened, as well as the provision of antiretroviral therapy to patients is improved.
HIV and AIDS - what are the differences?
The expressions HIV epidemic and AIDS epidemic are often used as equivalents. However, the difference between these terms is huge. HIV (human immunodeficiency virus) is an infection that affects the cells of the immune system, and AIDS (acquired immunodeficiency syndrome) is a consequence of its effect on the human body.
Currently, there is no medicine that can destroy HIV, and therefore, from the moment of infection, it is constantly present in the human body. In most cases, the disease begins unnoticed. Only after the incubation period, when the immune system begins to fight the virus, do the first signs of HIV infection appear. Enlarged lymph nodes, discomfort and pain in the throat when swallowing, diarrhea and increased body temperature are nonspecific symptoms that are often mistaken for a cold. When the first symptoms subside, a period of “calm” begins. It can last up to 15 years. At this time, the virus multiplies and gradually kills cells of the immune system, which leads to a pronounced decrease in immunity - the stage of AIDS. Severe viral and bacterial infections, fungal diseases, oncology - all this accompanies the immunodeficiency acquired as a result of HIV.

Influenza is an infectious disease that occurs with severe symptoms of intoxication (fever, headache, aches in muscles and joints) and is accompanied by damage to the mucous membranes of the respiratory tract.
The causative agents of influenza are viruses of types A, B, C. In this case, influenza type A causes the most severe forms of the disease.
The influenza virus epidemic remains one of the most pressing problems throughout the world, including Russia. The incidence rate depends both on the properties of the virus itself (virulence - the ability to cause disease) and on the strength of the population’s immunity.
Recent influenza epidemics have the following features:
- Simultaneous circulation of different influenza serotypes type A and B;
- Simultaneous circulation of influenza viruses and other respiratory viruses.
"Bird flu"
Avian influenza (H5N1) is an influenza virus that causes an infectious disease in birds, but has the ability to be transmitted from them to humans.
The disease was first described in Italy in 1880. In the 21st century, the infection spread to European countries (Austria and Germany, Sweden, the Czech Republic and Slovakia), as well as to South and North America and Africa through migratory birds. There is a virus in Russia bird flu discovered in 2005.
A person becomes infected with the virus from domestic waterfowl through droplets of their saliva or mucus. A contact route of infection is also possible.
The avian influenza virus is dangerous for humans, because the pathogen is extremely contagious and causes serious damage to the respiratory tract (pneumonia), liver and kidneys. It is resistant to the antiviral drug Remantadine, which complicates the treatment of the disease.

Swine flu (H1N1) is an infectious disease that affects the respiratory tract and is accompanied by fever.
At the end of the last century, the swine flu virus began to interact with avian and human flu, in other words, it mutated. The result was the now widely known subtype.
The first outbreaks of swine flu in humans were reported in Mexico in February 2009. Despite the fact that cases of infection have been recorded in at least 13 countries, the continent of North America, where the first influenza epidemic occurred, remains the most dangerous.
Treatment and prevention of swine flu is difficult. An effective vaccine has not yet been developed, and standard antiviral drugs do not guarantee a cure. The reason for this is the ability of the virus to mutate.
Influenza epidemic in Russia 2016-2017
The influenza virus epidemic in Russia began at the end of 2016 and continued at the beginning of 2017. According to forecasts, the morbidity structure is dominated by the Hong Kong influenza (H3N2), the pandemic of which swept across the globe in 1968-69.
Flu symptoms are characterized by severe intoxication:
- Fever above 39°C;
- Severe headache;
- Aches in muscles and joints;
- Chills;
- Pain, pain in the eyes, lacrimation;
- Nausea, vomiting, diarrhea;
- Dry cough.
Those at risk for developing the disease include: children, the elderly, pregnant women, and people suffering from chronic diseases.
During the flu season, if symptoms of a respiratory illness occur, you must see a doctor as soon as possible, because treatment should begin on the first day of illness. The most effective antiviral drugs are those that act directly on the virus (Oseltamivir).
Symptomatic treatment is no less important. When body temperature rises above 38.5°C, antipyretic drugs are indicated. To relieve a sore throat - antiseptic solutions for rinsing, lozenges and lozenges, sprays. To reduce dry cough - antitussive syrups and tablets.
To prevent an influenza epidemic, routine vaccination is carried out in advance of the season - September-October. Modern vaccines practically do not cause side effects, have a narrow list of contraindications, but they contain strains of influenza viruses that will be relevant according to WHO (World Health Organization) forecasts.

Children's infectious diseases: diphtheria, whooping cough, measles, scarlet fever, chicken pox - spread easily and quickly among children, causing epidemics in children's institutions. To stop the disease, restrictive measures are taken, which include quarantine and isolation of patients.
To prevent the occurrence of epidemics of childhood infections, vaccinations are carried out according to the national vaccination calendar. This preventative measure is the most effective and safe. In countries where vaccination coverage among children and adults reaches 90%, outbreaks of childhood infectious diseases are unlikely.
Measles epidemic
The incidence of measles in Russia is increasing from year to year. If earlier episodes of the disease were quite rare and were mainly caused by imported cases, now they are associated with the lack of immunity in the population against this infection. The first reports of a measles epidemic came from St. Petersburg. The disease subsequently spread to other regions of the country.
According to experts, the reason for the emergence of childhood infection in Russia (measles epidemic) is the refusal of many parents to vaccinate or anti-vaccination. The anti-vaccination movement disputes the safety of vaccinations, especially mass vaccinations. However, according to WHO (World Health Organization) experts, most of their arguments are not supported by facts.
The measles epidemic that broke out in Ireland in 1999-2000 is a striking example of an increase in incidence due to refusal to vaccinate. At the time, the national immunization rate was below 80%, and in North Dublin it was 60%.
Despite the fact that modern medicine has made great strides in the treatment of many diseases, there is still no etiotropic therapy for childhood infections. Complications of measles, especially those related to the central nervous system (CNS), respiratory tract and digestive system, are severe and can cause death. In order to prevent the spread of the measles epidemic in Russia, vaccination is recommended for all persons under 35 years of age.
Epidemics in the modern world
It would seem that science has reached such heights in modern world that epidemics of infectious diseases are simply impossible. However, this is not true. Viruses and bacteria mutate and adapt to changing conditions in order to survive. New viruses that are resistant to antiviral drugs and long-known bacteria that are no longer sensitive to antibiotics pose a real threat. In addition, military conflicts, humanitarian disasters, and the inability to comply with sanitary standards provoke the onset of epidemics, primarily of intestinal infections.

The outbreak of the Ebola virus epidemic began in the summer of 2014 in Central Africa. Then, in a short period of time, a dangerous infectious disease became known to the whole world.
The virus is transmitted from a sick person to a healthy person through direct contact with blood or other biological fluids. In African countries, the spread of the epidemic is facilitated by the customs of the inhabitants. They deliberately hide sick people from doctors, and bury the dead secretly, after washing the body. Graves are usually dug near settlements, next to running water.
The Ebola virus is characterized by the appearance of symptoms of intoxication (fever, pain in muscles and joints, sore throat) and a violation of the blood clotting process - a tendency to bleed. In many cases, the disease also manifests itself as damage to the kidneys and liver.
The end of the Ebola virus epidemic was recorded in December 2015. Although cases of the disease are still recorded in African countries.
Tuberculosis epidemic
Tuberculosis has been known since ancient times. Even the remains of Egyptian mummies retained signs of this infectious disease. However, the pathogen itself was discovered in 1882 by the German scientist Robert Koch. In honor of him, the microbe was named Koch's bacillus.
Tuberculosis infection occurs through airborne droplets. That is why the lungs are primarily affected, although bacteria can multiply in other organs - bones, skin, kidneys. With any localization of the process, the body as a whole suffers.
If a person becomes infected with the tuberculosis bacterium, this does not mean the disease will develop. The microbe can remain in the body for many years and not manifest itself, but when the immune system is weakened, it becomes activated.
The risk group for the development of tuberculosis includes children, pregnant and postpartum women, as well as people suffering from chronic diseases. A child's body only needs short contact with a source of infection to become ill. That is why vaccination is carried out already in the first days of the baby’s life.
Tuberculosis is considered an epidemic in Russia, which is gaining momentum. It is caused by several factors: bacterial resistance to many drugs and unfavorable living conditions of people.
Tuberculosis is considered a social disease. It affects people living in poverty. In our country, the development of the epidemic is facilitated by the deterioration in the standard of living of the population, the appearance of homeless people and refugees. In addition, for various reasons, Russian residents neglect preventive measures, which include annual fluorography. Only 30-40% of the population are screened regularly.
Epidemic of sexually transmitted diseases
According to the international classification of diseases, there are 9 infections that are predominantly sexually transmitted (venereal diseases). These include: syphilis, gonorrhea, chlamydia, trichomonas infection, genital herpes, papillomavirus infection and 3 more infectious diseases that are common in tropical countries and are not found in Russia.
In 1993, the strict system of clinical examination and registration of patients stopped working, and population migration began. This was the reason for the start of the epidemic of STIs (infections predominantly sexually transmitted) in Russia.
Combating an epidemic of sexually transmitted diseases is a difficult task. Primarily because many microbes no longer respond to antibacterial drugs and become resistant to them. For example, gonococcus, the infection that causes gonorrhea, is no longer sensitive to penicillin. The fact is that doctors of different specialties - dermatologists, gynecologists, urologists - use their own treatment regimens, which include prescribing a variety of antibiotics. This approach leads to mutation of the microbe and loss of sensitivity to drugs.
The spread of the epidemic can be stopped through preventive measures. First of all, this is educational work among the population. Until people are aware of the dangers of sexually transmitted diseases, they do not attach due importance to them. However, some sexually transmitted diseases (for example, genital herpes) remain in the human body forever and can be activated every month, causing suffering. Other infections can cause infertility or miscarriage.
Incredible facts
Few words in any language can cause as much horror, suffering and death as the word "plague." Indeed, infectious diseases have caused enormous harm to people for centuries. They destroyed entire nations, took more lives than even wars sometimes could, and also played a decisive role in the course of history.
Ancient people were no strangers to diseases. They encountered microbes that provoked the development of diseases in drinking water, food and the environment. Sometimes an outbreak of a disease could wipe out a small group of people, but this continued until people began to unite in populations, thereby allowing the infectious disease to become an epidemic. An epidemic occurs when a disease affects a disproportionate number of people within a particular population group, such as a city or geographic region. If the disease affects even more people, then these outbreaks become a pandemic.
People have also exposed themselves to new deadly diseases as a result of domesticating animals that carry equally dangerous bacteria. By coming into regular, close contact with previously wild animals, early farmers gave these microbes a chance to adapt to the human body.
In the process of man's exploration of more and more new lands, he came into close contact with microbes that he might never have encountered. By storing food, people attracted rats and mice into their homes, which brought even more germs. Human expansion led to the construction of wells and canals, which created the phenomenon of stagnant water, which was actively favored by mosquitoes and mosquito vectors various diseases. As technology developed, a particular type of microbe could easily be transported many kilometers from its original place of residence.
Epidemic 10: Smallpox
 Before the influx of European explorers, conquerors and colonists to the New World in the early 1500s, the American continent was home to 100 million indigenous people. In subsequent centuries, epidemic diseases reduced their number to 5-10 million. While these people, such as the Incas and Aztecs, built cities, they did not live in them long enough to catch as many diseases as the Europeans "owned", nor did they domesticate as many animals. When Europeans arrived in America, they brought with them many diseases for which the indigenous people had no immunity or protection.
Before the influx of European explorers, conquerors and colonists to the New World in the early 1500s, the American continent was home to 100 million indigenous people. In subsequent centuries, epidemic diseases reduced their number to 5-10 million. While these people, such as the Incas and Aztecs, built cities, they did not live in them long enough to catch as many diseases as the Europeans "owned", nor did they domesticate as many animals. When Europeans arrived in America, they brought with them many diseases for which the indigenous people had no immunity or protection.
Chief among these diseases was smallpox, caused by the variola virus. These microbes began attacking humans thousands of years ago, with the most common form of the disease boasting a mortality rate of 30 percent. Symptoms of smallpox include high fever, body aches and a rash that appears as small, fluid-filled boils. The disease primarily spreads through direct contact with the skin of an infected person or through body fluids, but can also be transmitted through airborne droplets in confined spaces.
Despite the development of a vaccine in 1796, the smallpox epidemic continued to spread. Even as recently as 1967, the virus has killed more than two million people, and millions of people around the world have been severely affected by the disease. That same year, the World Health Organization launched aggressive efforts to eradicate the virus through mass vaccination. As a result, the last case of smallpox infection was recorded in 1977. Now effectively removed from the natural world, the disease exists only in laboratories.
Epidemic 9: 1918 Influenza
 The year was 1918. The world watched as the First world war was coming to an end. By the end of the year, the death toll is estimated to reach 37 million worldwide. It was then that a new disease appeared. Some call it the Spanish Flu, others the Great Flu or the 1918 Flu. Whatever it is called, this disease destroyed 20 million lives within a few months. A year later, the flu would moderate its ardor, but irreparable damage had nevertheless been done. According to various estimates, the number of victims was 50-100 million people. This flu is considered by many to be the worst epidemic and pandemic ever recorded in history.
The year was 1918. The world watched as the First world war was coming to an end. By the end of the year, the death toll is estimated to reach 37 million worldwide. It was then that a new disease appeared. Some call it the Spanish Flu, others the Great Flu or the 1918 Flu. Whatever it is called, this disease destroyed 20 million lives within a few months. A year later, the flu would moderate its ardor, but irreparable damage had nevertheless been done. According to various estimates, the number of victims was 50-100 million people. This flu is considered by many to be the worst epidemic and pandemic ever recorded in history.
In fact, the 1918 flu was not the typical virus we encounter every year. It was a new strain of influenza virus, avian influenza virus AH1N1. Scientists suspect the disease jumped from birds to humans in the American West shortly before the outbreak. Later, as influenza killed more than 8 million people in Spain, the disease was named the Spanish flu. Around the world, people's immune systems were not prepared for the attack of a new virus, just as the Aztecs were not prepared for the "arrival" of smallpox in the 1500s. Massive transportation of soldiers and food towards the end of the First World War allowed the virus to quickly “organize” a pandemic and reach other countries and continents.
The 1918 flu was accompanied by symptoms of the common flu, including fever, nausea, pain and diarrhea. In addition, patients often developed black spots on their cheeks. Because their lungs were filled with fluid, they risked dying from lack of oxygen, and many did.
The epidemic subsided within a year as the virus mutated into other, safer forms. Most people today have developed some immunity to this family of viruses, inherited from those who survived the pandemic.
Outbreak 8: Black Death
 The Black Death is considered the first plague pandemic, killing half the population of Europe in 1348 and also wiping out parts of China and India. This disease destroyed many cities, constantly changed the structure of classes, and affected global politics, commerce and society.
The Black Death is considered the first plague pandemic, killing half the population of Europe in 1348 and also wiping out parts of China and India. This disease destroyed many cities, constantly changed the structure of classes, and affected global politics, commerce and society.
The Black Death was long thought to be a plague that traveled in bubonic form on rat fleas. Recent research has cast doubt on this claim. Some scientists now argue that the Black Death may have been a hemorrhagic virus similar to Ebola. This form of the disease leads to enormous blood loss. Experts continue to examine the remains of plague victims in the hope of finding genetic evidence to substantiate their theories.
Still, if it was a plague, then the Black Death is still with us. Caused by the bacterium Yersinia Pestis, the disease can still live in poor regions where rats are heavily populated. Modern medicine makes it easy to treat the disease in its early stages, so the threat of death is much lower. Symptoms include swollen lymph nodes, fever, cough, bloody sputum and difficulty breathing.
Epidemic 7: Malaria
 Malaria is far from new to the world of epidemics. Its impact on human health dates back more than 4,000 years ago, when Greek writers noted its effects. Mention of the mosquito-borne disease can also be found in ancient Indian and Chinese medical texts. Even then, doctors were able to make a vital connection between the disease and stagnant water in which mosquitoes and mosquitoes breed.
Malaria is far from new to the world of epidemics. Its impact on human health dates back more than 4,000 years ago, when Greek writers noted its effects. Mention of the mosquito-borne disease can also be found in ancient Indian and Chinese medical texts. Even then, doctors were able to make a vital connection between the disease and stagnant water in which mosquitoes and mosquitoes breed.
Malaria is caused by four species of the microbe Plasmodium, which is “common” to two species: mosquitoes and humans. When an infected mosquito decides to feast on human blood and succeeds, it transfers the microbe to the human body. Once the virus is in the blood, it begins to multiply inside red blood cells, thereby destroying them. Symptoms range from mild to fatal and typically include fever, chills, sweating, headaches and muscle aches.
Specific figures on the consequences of the first outbreaks of malaria are difficult to find. However, it is possible to trace the impact of malaria on humans by studying the regions affected by the disease. In 1906, the United States employed 26,000 people to build the Panama Canal; after some time, more than 21,000 of them were hospitalized with a diagnosis of malaria.
In the past, during wartime, many troops often experienced severe casualties due to outbreaks of malaria. According to some estimates, during the American Civil War, more than 1,316,000 people suffered from this disease, and more than 10,000 of them died. During World War II, malaria incapacitated British, French and German troops for three years. Nearly 60,000 American soldiers died from the disease in Africa and the South Pacific during World War II.
Towards the end of World War II, the United States attempted to stop the malaria epidemic. The country initially made huge strides in this area through the use of now-banned insecticides, followed by preventive measures to keep the mosquito population low. After the Center for Disease Control in the United States declared that malaria had been eliminated in the country, the World Health Organization actively began to fight the disease throughout the world. The results were mixed, however, the cost of the project, war, the emergence of a new type of drug-resistant malaria and insecticide-resistant mosquitoes ultimately led to the abandonment of the project.
Today, malaria still poses a problem in most countries of the world, especially in sub-Saharan Africa, as they were excluded from the WHO eradication campaign. Each year, up to 283 million cases of malaria are recorded and more than 500,000 people die.
However, it is important to add that compared to the beginning of the 21st century, the number of cases and deaths today has decreased significantly.
Epidemic 6: Tuberculosis
 Tuberculosis has ravaged the human population throughout history. Ancient texts detail how victims of the disease withered away, and DNA testing revealed the presence of tuberculosis even in Egyptian mummies. Caused by the bacterium Mycobacterium, it is transmitted from person to person through airborne transmission. The bacterium usually attacks the lungs, resulting in chest pain, weakness, weight loss, fever, excessive sweating and a bloody cough. In some cases, the bacterium also affects the brain, kidneys, or spine.
Tuberculosis has ravaged the human population throughout history. Ancient texts detail how victims of the disease withered away, and DNA testing revealed the presence of tuberculosis even in Egyptian mummies. Caused by the bacterium Mycobacterium, it is transmitted from person to person through airborne transmission. The bacterium usually attacks the lungs, resulting in chest pain, weakness, weight loss, fever, excessive sweating and a bloody cough. In some cases, the bacterium also affects the brain, kidneys, or spine.
Beginning in the 1600s, a European tuberculosis epidemic known as the Great White Plague raged for more than 200 years, killing one in seven people infected. Tuberculosis was a persistent problem in Colonial America. Even in the late 19th century, 10 percent of all deaths in the United States were due to tuberculosis.
In 1944, doctors developed the antibiotic streptomycin, which helped fight the disease. In subsequent years, even more significant breakthroughs were made in this field and, as a result, after 5,000 years of suffering, humanity was finally able to cure what the ancient Greeks called “the wasting disease.”
However, despite modern treatments, tuberculosis continues to affect 8 million people every year, with 2 million deaths. The disease returned in a big way in the 1990s, thanks largely to global poverty and the emergence of new antibiotic-resistant strains of tuberculosis. In addition, patients with HIV/AIDS have a weakened immune system, making them more susceptible to tuberculosis infection.
Epidemic 5: Cholera
 People in India have lived with the risk of cholera since ancient times, but this danger did not manifest itself until the 19th century when the rest of the world encountered the disease. During this period of time, traders unintentionally exported the deadly virus to cities in China, Japan, North Africa, the Middle East and Europe. There have been six recorded cholera pandemics that have killed millions of people.
People in India have lived with the risk of cholera since ancient times, but this danger did not manifest itself until the 19th century when the rest of the world encountered the disease. During this period of time, traders unintentionally exported the deadly virus to cities in China, Japan, North Africa, the Middle East and Europe. There have been six recorded cholera pandemics that have killed millions of people.
Cholera is caused by an E. coli bacteria called Vibrio cholerae. The disease itself is usually very mild. Five percent of those who contract the disease experience severe vomiting, diarrhea and cramps, with these symptoms leading to rapid dehydration. As a rule, most people cope with cholera easily, but only when the body is not dehydrated. People can become infected with cholera through close physical contact, but cholera is primarily spread through contaminated water and food. During the Industrial Revolution in the 1800s, cholera spread to major cities in Europe. Doctors insisted on "clean" living conditions and the creation of improved sewage systems, believing that the epidemic was caused by " bad air"However, this actually helped, as cholera cases dropped significantly after the purified water supply was adjusted.
For decades, cholera seemed to be becoming a thing of the past. However, a new strain of cholera emerged in 1961 in Indonesia and eventually spread to much of the world. In 1991, about 300,000 people were affected by the disease and more than 4,000 died.
Epidemic 4: AIDS
 The emergence of AIDS in the 1980s led to a global pandemic, killing more than 25 million people since 1981. According to the latest statistics, there are currently 33.2 million HIV-infected people living on the planet. AIDS is caused by the human immunodeficiency virus (HIV). The virus spreads through contact with blood, semen and other biological material, causing irreparable damage to the human immune system. A damaged immune system opens the door to infections called opportunistic infections, which to an ordinary person don't cause any problems. HIV becomes AIDS if the immune system is damaged sufficiently.
The emergence of AIDS in the 1980s led to a global pandemic, killing more than 25 million people since 1981. According to the latest statistics, there are currently 33.2 million HIV-infected people living on the planet. AIDS is caused by the human immunodeficiency virus (HIV). The virus spreads through contact with blood, semen and other biological material, causing irreparable damage to the human immune system. A damaged immune system opens the door to infections called opportunistic infections, which to an ordinary person don't cause any problems. HIV becomes AIDS if the immune system is damaged sufficiently.
Scientists believe the virus jumped from monkeys to humans in the mid-20th century. During the 1970s, Africa's population grew significantly, and war, poverty and unemployment plagued many cities. Thanks to prostitution and intravenous drug use, HIV has become very easy to spread through unprotected sex and the reuse of contaminated needles. Since then, AIDS has traveled south of the Sahara, leaving millions of children orphaned and depleting the workforce in many of the world's poorest countries.
There is currently no cure for AIDS, however, there are some drugs that can prevent HIV from developing into AIDS, and additional drugs can also help fight opportunistic infections.
Epidemic 3: Yellow fever
 When Europeans began “importing” African slaves to America, they also brought with them, in addition to a number of new diseases, yellow fever. This disease destroyed entire cities.
When Europeans began “importing” African slaves to America, they also brought with them, in addition to a number of new diseases, yellow fever. This disease destroyed entire cities.
When French Emperor Napoleon sent an army of 33,000 French soldiers to North America, yellow fever killed 29,000 of them. Napoleon was so shocked by the number of casualties that he decided that this territory was not worth such losses and risks. France sold the land to the United States in 1803, an event that would go down in history as the Louisiana Purchase.
Yellow fever, like malaria, is transmitted from person to person through mosquito bites. Typical symptoms include fever, chills, headache, muscle pain and vomiting. The severity of symptoms ranges from mild to fatal, and severe infection can lead to bleeding, shock, and severe kidney and liver failure. Kidney failure causes jaundice and yellowing of the skin, which gives the disease its name.
Despite vaccinations and improved treatment methods, the epidemic still flares up periodically in South America and Africa.
Epidemic 2: Typhus
 The tiny microbe Rickettsia prowazekii is responsible for one of the world's most devastating infectious diseases: typhus.
The tiny microbe Rickettsia prowazekii is responsible for one of the world's most devastating infectious diseases: typhus.
Humanity has been suffering from the disease for centuries, with thousands of people falling victim to it. Given the fact that the disease often affected military personnel, it was called "camp fever" or "war fever." During the 30 Years' War in Europe (1618-1648), typhoid, plague and famine killed 10 million people. Sometimes outbreaks of typhus dictated the outcome of the entire war. For example, when Spanish troops laid siege to the Moorish fortress of Granada in 1489, a typhoid outbreak immediately killed 17,000 soldiers within a month, leaving a force of 8,000 men. Due to the ravages of typhus, another century passed before the Spaniards were able to drive the Moors out of their state. Also during World War I, the disease claimed several million lives in Russia, Poland and Romania.
Symptoms of a typhus epidemic usually include headache, loss of appetite, malaise and a rapid rise in temperature. This quickly develops into a fever, accompanied by chills and nausea. If left untreated, the disease affects blood circulation, which can result in gangrene, pneumonia and kidney failure.
Improved treatment methods and sanitation have greatly reduced the likelihood of typhoid epidemics in the modern era. The advent of the typhus vaccine during World War II helped effectively eradicate the disease in the developed world. However, outbreaks are still occurring in parts of South America, Africa and Asia.
Epidemic 1: Poliomyelitis
 Researchers suspect that polio has plagued humanity for thousands of years, paralyzing and killing thousands of children. In 1952, there were an estimated 58,000 cases of polio in the United States, with one third of patients paralyzed and more than 3,000 deaths.
Researchers suspect that polio has plagued humanity for thousands of years, paralyzing and killing thousands of children. In 1952, there were an estimated 58,000 cases of polio in the United States, with one third of patients paralyzed and more than 3,000 deaths.
The cause of the disease is poliovirus, which targets the human nervous system. The virus is often spread through contaminated water and food. Initial symptoms include fever, fatigue, headache, nausea, with one in 200 cases resulting in paralysis. Although the disease usually affects the legs, sometimes the disease spreads to the respiratory muscles, which is usually fatal.
Polio is common in children, but adults are also susceptible to the disease. It all depends on when a person first encounters the virus. The immune system is better prepared to fight the disease at an early age, so the older the person who is first diagnosed with the virus, the higher the risk of paralysis and death.
Poliomyelitis has been known to man since ancient times. Over time, especially in children, the immune system strengthened and began to better respond to the course of the disease. During the 18th century, sanitary conditions improved in many countries. This limited the spread of the disease, while there was a decrease in immune resistance, and the chances of contracting it at a young age gradually disappeared. As a result, more people were exposed to the virus at an older age, and the number of cases of paralysis in developed countries increased sharply.
To date, there is no effective medicinal product against polio, but doctors are constantly improving the vaccine, which was released in the early 1950s. Since then, the number of polio cases in the United States and other developed countries has declined sharply, and only a small number developing countries still suffer from frequent polio epidemics. Since humans are the only carriers of the virus, widespread vaccination guarantees almost complete eradication of the disease.
Observing a bewildering variety of deadly fevers over the centuries, medical scientists have tried to associate typical patterns of infectious diseases with specific causes, in order to identify and classify diseases on this basis, and then develop specific methods to counteract them. Considering the evolution of our knowledge about some of the main epidemic diseases, we can trace the formation of the modern understanding of the epidemic.
Plague. In the Middle Ages, plague epidemics were so devastating that the name of this particular disease figuratively became synonymous with all sorts of misfortunes. The successive plague pandemics of the 14th century. killed a quarter of the then population of Europe. The quarantine isolation of travelers and arriving ships was futile.
It is now known that plague is a disease of wild rodents, particularly rats, which is transmitted by Xenopsyllacheopis fleas. These fleas infect people living in close proximity to infected rats, the reservoir of infection. With bubonic plague, transmission of infection from person to person begins only with the development of the highly contagious pulmonary form of the disease in the patient.
At the end of the 17th century. the plague disappeared from Europe. The reasons for this are still unknown. It is assumed that with changes in living conditions in Europe, the population began to live further from reservoirs of infection. Due to the lack of wood, houses began to be built from brick and stone, which is to a lesser extent than wooden buildings old type, suitable for rats.
Cholera. In the 19th century cholera pandemics occurred in most countries of the world. In the classic study of the London physician J. Snow, the water route of transmission of infection during the cholera epidemic of 1853–1854 was correctly identified. He compared the number of cholera cases in two neighboring areas of the city that had different sources water supplies, one of which was contaminated with sewage. Thirty years later, the German microbiologist R. Koch, using microscopy and bacterial cultivation methods to identify the causative agent of cholera in Egypt and India, discovered the “cholera comma,” later called Vibrio cholerae (Vibriocholerae).
Typhus. The disease is associated with unsanitary living conditions, usually during war. It is also known as camp, prison or ship fever. When in 1909 the French microbiologist C. Nicole showed that typhus is transmitted from person to person by body lice, its connection with overcrowding and poverty became clear. Knowing how the infection is transmitted allows health workers to stop the spread of epidemic (lice) typhus by spraying insecticidal powder on the clothing and body of those at risk of infection.
Smallpox. Modern vaccination as a method of preventing infectious diseases was developed based on the early successes achieved by medicine in the fight against smallpox by immunizing (vaccinating) susceptible individuals. To administer the vaccine, fluid from a smallpox blister of a patient with an active infection was transferred to a scratch on the skin of the immunized person's shoulder or hand. If lucky, a mild illness occurred, leaving lifelong immunity after recovery. Sometimes immunization caused the development of a typical disease, but the number of such cases was so small that the risk of vaccination complications remained quite acceptable.
Immunization began to be used in Europe in 1721, but long before that it was used in China and Persia. It was thanks to her that by 1770 smallpox ceased to occur in the wealthy sections of the population.
The credit for further improvement of smallpox immunization belongs to a rural doctor from Gloucestershire (England) E. Jenner, who drew attention to the fact that people who had mild cowpox do not get smallpox, and suggested that cowpox creates immunity to human smallpox.
At the beginning of the 20th century. smallpox vaccine became readily available throughout the world due to its mass production and cold storage. The latest chapter in the history of smallpox was marked by a mass vaccination campaign carried out in all countries by the World Health Organization.
Yellow fever. In the 18th–19th centuries. Among the epidemic diseases of the Western Hemisphere, yellow fever occupied a prominent place in the United States, as well as in the countries of Central America and the Caribbean. Doctors, who assumed that the disease was transmitted from person to person, demanded the isolation of the sick to combat the epidemic. Those who linked the origin of the disease with atmospheric pollution insisted on sanitary measures.
In the last quarter of the 19th century. yellow fever began to be associated with mosquito bites. In 1881, the Cuban doctor K. Finlay suggested that the disease was transmitted by Aëdesaegypti mosquitoes. Evidence of this was presented in 1900 by the yellow fever commission working in Havana, headed by W. Reed (USA).
The implementation of the mosquito control program over the coming years contributed not only to a significant reduction in the incidence of disease in Havana, but also to the completion of construction of the Panama Canal, which was almost stopped due to yellow fever and malaria. In 1937, a doctor from the Republic of South Africa, M. Theiler, developed an effective vaccine against yellow fever, more than 28 million doses of which were produced by the Rockefeller Foundation from 1940 to 1947 for tropical countries.
Polio. Paralytic poliomyelitis (infantile paralysis) appeared as an epidemic disease at the turn of the 19th and 20th centuries. It is amazing that in underdeveloped countries with poor, unsanitary living conditions, the incidence of polio has remained low. At the same time, in highly developed countries, on the contrary, epidemics of this disease began to occur with increasing frequency and severity.
The key to understanding the epidemic process in polio was the concept of asymptomatic carriage of the pathogen. This type of latent infection occurs when a person, having become infected with the virus, acquires immunity in the absence of any symptoms of the disease. Carriers, while remaining healthy themselves, can shed the virus, infecting others. It has been found that in conditions of poverty and crowded living conditions, the likelihood of contact with the virus increases sharply, as a result of which children become infected with polio very early, but the disease manifests itself quite rarely. The epidemic process proceeds as an endemic, secretly immunizing the population, so that only isolated cases of infantile paralysis occur. In countries with a high standard of living, such as North America and Northern Europe, there was a marked rise in the incidence of paralytic polio from the 1900s to the 1950s.
The polio virus was isolated by K. Landsteiner and G. Popper already in 1909, but methods for preventing the disease were found only much later. Three serotypes (i.e., types present in the blood serum) of polioviruses have been identified, and strains of each of them were found in 1951 to be able to reproduce in tissue culture. Two years later, J. Salk reported his method of inactivating the virus, which made it possible to prepare an immunogenic and safe vaccine. The long-awaited inactivated Salk vaccine became available for mass use in 1955.
The polio epidemic in the United States has stopped. Since 1961, a live attenuated vaccine developed by A. Seibin began to be used for mass immunization against polio.
AIDS. In 1981, when acquired immunodeficiency syndrome (AIDS) was first described as a distinct clinical entity, its causative agent was not yet known. The new disease was initially recognized only as a syndrome, i.e. combination of characteristic pathological symptoms. Two years later, it was reported that the basis of the disease was the suppression of the body's immune system by a retrovirus, which was called the human immunodeficiency virus (HIV). Patients develop increased susceptibility to a variety of infectious pathogens, which manifests itself clinically only in the later stages of HIV infection, but initially the disease can remain in the incubation period for a very long time, up to 10 years.
The first cases were homosexual men, then there were reports of transmission of the infection through transfusion of blood and its components. Subsequently, the spread of HIV infection was identified among injecting drug users and their sexual partners. In Africa and Asia, AIDS is transmitted primarily through sexual contact. Currently, the disease is spreading throughout the world, becoming an epidemic.
Ebola fever. Ebola virus as the causative agent of African hemorrhagic fever was first identified in 1976 during an epidemic in southern Sudan and the north of the Republic of Zaire. The disease is accompanied by high fever and profuse bleeding; the mortality rate in Africa exceeds 50%. The virus is transmitted from person to person through direct contact with infected blood or other body secretions. Often infected medical staff, to a lesser extent, household contacts contribute to the spread of infection. The reservoir of infection is still unknown, but it may be monkeys, which is why strict quarantine measures have been introduced to prevent the import of infected animals.
To make it clearer, the word “epidemic” is translated from Greek as “a general disease among the people.” An epidemic cannot be considered an outbreak of a disease that has spread throughout the country and not in certain regions. Fortunately, advances in medicine have reduced the risk of epidemics and pandemics to a minimum. Among the current epidemics, the most common are influenza and ARVI epidemics; one rarely hears about a plague epidemic, since doctors are actively taking measures to protect against diseases among the population.
The worst epidemics in history
Epidemics have occurred in human history since ancient times. Diseases devastated entire cities; corpses of people who died from diseases lay on the streets. Medicine had so much low level development that could not withstand outbreaks of plague, malaria or cholera, create required level security. Let's get acquainted with the most terrible epidemics that are written down in black pages in the history of mankind.
In 541-542 BC. The bubonic plague broke out in the Byzantine Empire. In terms of its consequences, it was later compared to the wave of the Black Death in Europe, when every third European died from the disease. At the same time, Byzantium became part of a general pandemic that swept the whole world - North Africa and America, Asia and Europe were affected. For 200 years, the disease raged in these areas of the globe. Historians still cannot calculate even the approximate number of deaths.
The period in world history from 1665 to 1666 will be remembered by the British as the Great Plague of London. About 100 thousand people died - this is a fifth of the population of the entire city. The bubonic plague, as it was later established, broke out due to unsanitary conditions. In its consequences, the epidemic can be compared with the Black Death, which broke out from 1347 to 1353 - then more than 25 million people died.
The Black Death, also called the Great or Bubonic Plague, is the worst plague epidemic in world history. The pandemic began in the mid-1320s in Asia and spread throughout the world within a few years, largely due to traders and soldiers. The Black Death began its march across Europe, arriving in Crimea in 1340. Among Europeans alone, about 30 million people died from the Black Death. With each generation, the plague returned until the early eighteenth century.
Another tragic story, this time in the Russian chronicle, occurred at the end of 1770 in Moscow, when the plague epidemic broke out. It all started with several cases of illness and ended tragically. The Russian authorities failed to cope with the dangerous disease - instead of taking competent measures, the houses of those families where the patient was located were burned down, public baths were closed to avoid the spread of lice.
On September 17, 1771, the Plague Riot broke out - only after it did the authorities begin to ensure the fight against the plague.
Plague - greetings from the Middle Ages
Epidemics of the Middle Ages were associated with mass plague diseases. The danger was that the plague chronicle of which is described above was not amenable to medical treatment - the practical level of doctors was low. In 1998, it was established that the cause of the Black Death was the plague bacillus; according to data for 2013 and 2014, there were no dangerous outbreaks of the disease. Among the causes of the terrible epidemic, which claimed a total of 60 million people, are:
- environmental factor - a sharp change from cold to warm climate,
- raging civil wars and other military conflicts,
- poverty and vagrancy of the population,
- low level or complete absence of personal hygiene, violation of sanitary safety measures,
- terrible sanitary condition of cities,
- a huge number of rats that spread the disease.
Characteristics of the plague epidemic
At a minimum, the main danger of any epidemic is the rapid spread of the disease and a large number of deaths. The plague occurs exclusively in severe form; lice, rats, fleas and even cats can spread it. The most common plagues are bubonic and pneumonic. Now the development of medicine makes it possible to prevent death from plague in 95% of cases, whereas previously almost every case was fatal. Not so long ago, by historical standards, the plague raged on Far East- 100 thousand people became victims of the epidemic.
According to data for 2015, the number of people infected with the plague annually is about 2.5 thousand. Unfortunately, there is no trend towards disappearance or reduction in the level of the disease. The plague has not appeared in Russia since 1979. Modern outbreaks of plague were recorded in 2013 and 2014 in Madagascar, killing 79 people.
Flu - information and symptoms
Until now, the flu epidemic claims the lives of 250 to 500 thousand people every year, according to data for 2013-2014. The influenza virus is predominantly fatal to older people over 65 years of age. In many countries, including Russia, preventive measures are being taken to prevent an influenza epidemic. Moreover, the virus is relatively young - in separate group it was identified in the 30s of the twentieth century, before that the Spanish flu was rampant in Europe.
The Spanish flu epidemic is considered the worst in history. Occurred in 1918-1919, a wave of diseases swept across the world, eventually 550 million people were infected, of which 100 million people died. The influenza epidemic owes its appearance to the First World War, and at the same time managed to surpass the war in terms of the number of victims. The Spanish flu was characterized by a blue complexion and a bloody cough for the patient.
In the first weeks of its spread alone, the Spanish flu killed 25 million people.
Emergence of a measles epidemic
A measles epidemic is an outbreak of a disease that is a leading cause of death in infants. Measles is also difficult for adults to tolerate. In 2011 alone, 158 thousand people became victims of this insidious disease. Most of them are children under 5 years of age. Measles is dangerous because it spreads by airborne droplets, while the sick person himself also becomes infectious, and the people around him cannot think about safety.
Measles can appear in adults if a person was not vaccinated as a child or did not have it. Then the body develops immunity against measles. Adults with measles feel seriously ill - the disease is accompanied by pneumonia and other complications. It is especially dangerous for people with immunodeficiency to catch measles - death for such patients is almost inevitable. Measles epidemics occurred in different countries around the world in 2013 and 2014.